EMR Phase 2.1 – what does it mean for clinical nursing/midwifery documentation?
Clinical documentation has always been a vital Nursing and Midwifery role. Accurate and timely clinical documentation aids in the communication of critical clinical information within and between teams, and enables episodes of care to be summarised for safe and efficient handover and discharge to primary and community care.
Clinical documentation also aids in clinical coding, drives funding and research, informs service planning and is used for clinical incident investigations and legal proceedings.
Western Health’s EMR Phase 1, including optimisation projects and uplifts, was the beginning of our digital journey. It has changed the way that nurses and midwives document clinical care for the majority of our inpatient areas – now it’s time to extend this change to other parts of the organisation.
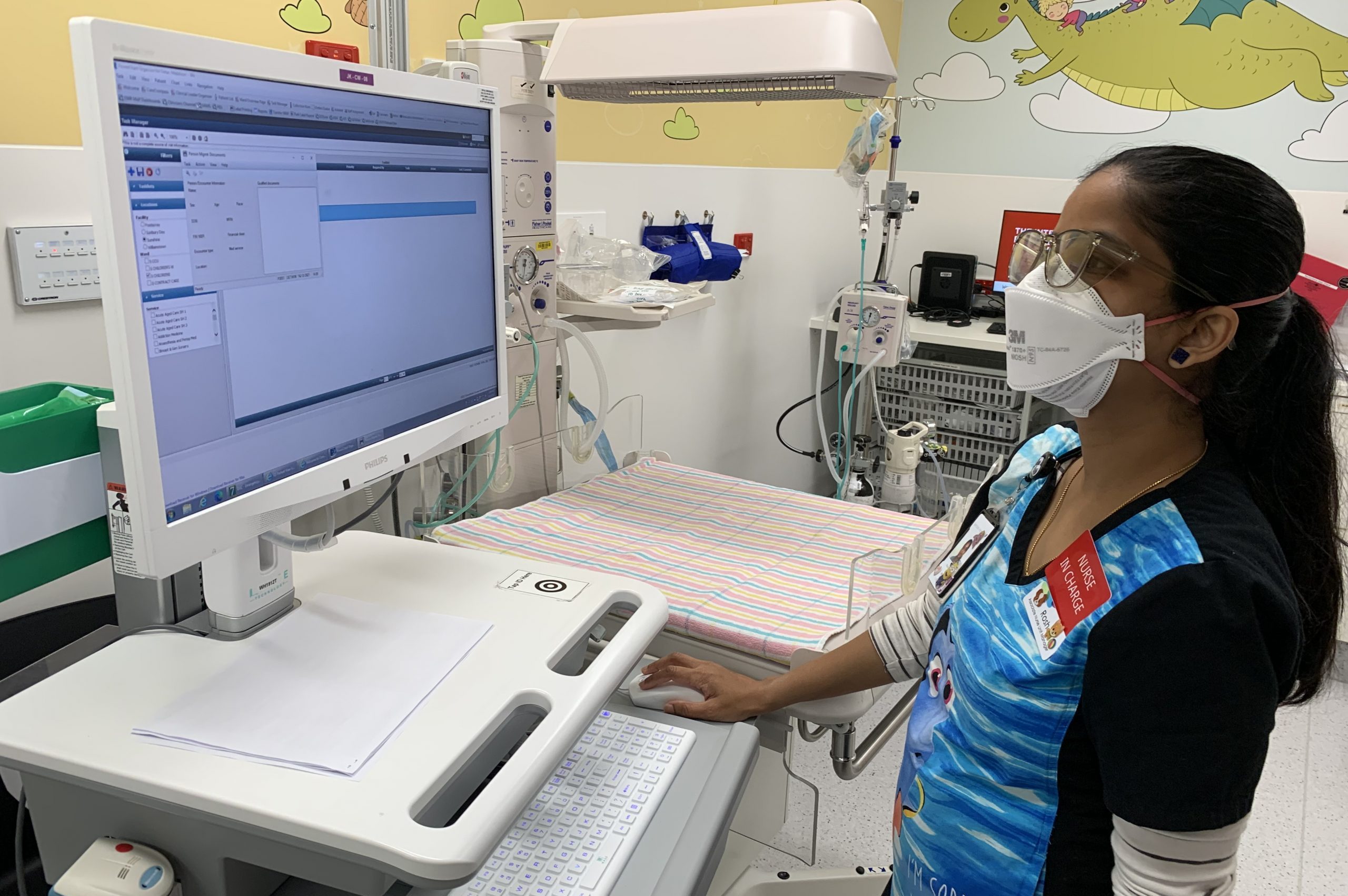
From Go-Live of EMR Phase 2.1 in July 2023, nurses and midwives working in Emergency, Perioperative Services, Critical Care & ICU, Women’s & Children’s, Outpatient Clinics and Cancer Services will complete their clinical documentation in the EMR. Future phases of the EMR will complete the transition to a fully integrated system.
Having all clinical documentation completed in a single system is an important part of achieving a seamless electronic patient journey – facilitating safe and effective patient care, reducing clinical risk and improving efficiency. Here are some of the benefits of integrated nursing/midwifery documentation:
- In our Emergency departments, a Behaviours of Concern (BOC) assessment is completed during triage. A BOC score greater than 2 will trigger a BOC alert on LaunchPoint – the ED tracking board that will be used to track, manage and monitor patients in the department
- In Women’s & Children’s, triage documentation in Maternity Assessment Centre will be viewable by clicking on an icon on the Maternity Tracking Board. Documentation for expressed breast milk will be completed in the EMR ensuring greater visibility of information and features which support positive patient ID
- Patient notes in outpatient clinics will be documented in the EMR and viewable by clinicians across the organisation
- In Cancer Services, documentation of Chemotherapy Patient Education will be standardised and viewable by all clinicians involved in the patient’s care
For further information please contact the Nursing and Midwifery Informatics Team, Kate Renzenbrink –Kate.Renzenbrink@wh.org.au and Kylee Ross – Kylee.Ross@wh.org.au
